If you’re older than 30, your skeleton’s already rebelling, tossing out bone faster than you can replace it. As doctors deliberate over when to begin osteoporosis treatments, your best bet is to get serious about diet and exercise. May is Osteoporosis Month, so it's time to bone up on how to hang onto your main frame.
We’ve all seen elderly people with humped backs or heard stories about grandparents who fell and broke their hips. Some of us even know women in their 50s who break a rib working out or moving furniture, only to learn they have osteoporosis, a loss of bone that leads to debilitating bone fractures.
Osteoporosis is a major health threat for aging females: About 8 million of the 10 million osteoporosis sufferers in the U.S. are women. Another 34 million have osteopenia, a precursor to the disease. And one in three women over 50 get fractures resulting from osteoporosis.
What Bone Loss Looks Like
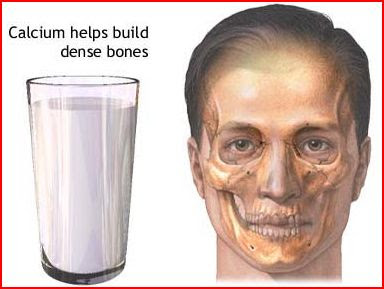
Bone is not just a solid hunk of calcium; it’s living, growing tissue with a soft core and a hardened framework of calcium phosphate. The inner core, or marrow, produces our blood cells. And bones (along with teeth) act as a storage tank for more than 99% of the body’s calcium.
As a living organ, bone is constantly breaking down its older framework and replacing it. Formation outpaces destruction until about age 30. After that, destruction slowly overtakes formation, causing a net bone loss.
As the loss becomes severe, bones lose density, becoming more porous and fragile. In fact, under a microscope, osteoporotic bone looks like a sponge. The weakened bone, like a dry twig, becomes more vulnerable to fractures, even under normal stresses.
That’s one reason grandma hunches over like she’s perennially searching for a dropped penny. The hump on the back of the elderly – called the dowager’s hump because it occurs mostly in women – results from small bone fractures on the front of the vertebrae, usually upper ones. As the fractured edge of a vertebra compresses, the vertebrae above it shift forward, curving the spine. The spine’s forward tip results in a hump, or kyphosis (which means "bent over").
As more vertebrae crack or collapse, the hump becomes more pronounced and painful, limiting activities as well: A woman may have to crane her neck to look someone in the face and breathing becomes more difficult because the new spinal position makes it harder for the lungs to expand.
Other common results of osteoporosis are fractures of the hip and wrists in a fall. Hip fractures – 300,000 per year – are the most serious. About 24% of hip-fracture patients – and a third of elderly men with hip fractures – die within a year, often because they can’t regain mobility.
Women are particularly vulnerable: Their bone loss accelerates in the first few years after menopause as estrogen, which stimulates bone growth, declines. Small, thin-boned women are at greatest risk. Other factors include:
- Caucasian or Asian ancestry
- Family history of osteoporosis
- Anorexia
- Low calcium and vitamin D intake
- Long-term use of steroids
- Cigarette smoking
- Alcoholism
- Inactivity
When Bone Loss Becomes a Problem
As with many trends in medicine, the prevailing wisdom on bone loss is shifting. This is affecting recommendations on when bone-loss treatments should begin.
Normal bone mass is defined as the average bone mineral density of a white woman between 20 and 29 years old. Based on that, researchers developed a T-score: A zero score was baseline (ideal), anything between zero and negative 1 was normal; negative 2.5 or lower indicated osteoporosis.
But scores between negative 1 and negative 2.5 fell into a grey area called osteopenia, which involves low bone density and mass. It became a catch phrase for bone density scores falling outside the "normal" range.
In 2004, the National Osteoporosis Foundation (NOF) and the American College of Obstetrics and Gynecology (ACOG) advised women who scored negative 2.0 or lower (or negative 1.5 or lower if they had certain risk factors such as family history, smoking etc.) should get osteoporosis treatment.
That shift increased the number of aged 65-plus women recommended for treatment from 6.5 million to 11 million. For women 50 to 64 years old, the treatment group expanded from 1.6 million to 4 million.
Now women’s health experts question whether those diagnosed with osteopenia need medical treatment. The medications are expensive and can have significant side effects, such as chest pain severe joint, bone or muscle pain or heartburn.
The new standard raised questions: How much would the extension of treatment reduce serious fractures? At what point along the continuum of bone loss – from osteopenia to osteoporosis – should treatment begin and when do the benefits outweigh the cost and risks?
Your Bone-Saving Options
Fortunately, you don’t have to wait for doctors to weigh in to protect yourself. Here are seven ways to strengthen your bones:
1. Eat for better bones. Bulk up on foods high in calcium and vitamin D. Calcium is the major bone builder, but it needs vitamin D to do its job. Vitamin D helps the body absorb calcium that would otherwise flush out in our urine. Foods high in calcium include dairy products, tofu, sardines, salmon, turnips and leafy greens. Foods high in vitamin D: salmon, tuna and other saltwater fish, fortified milk, egg yolks, liver and fish oils.
2. Get some daily sun. Sunlight stimulates the production of vitamin D in our skin. So get about five to 30 minutes of sun – without sunscreen – at least twice a week. (But don’t overdo it because too much sun raises the risk of skin cancer.)
3. Exercise. Just like muscles, bones need exercise to stay healthy. Strength training with weight-bearing exercises (such as walking, jogging and dancing) helps prevent or slow progression of osteoporosis. Strength-training increases the tug of muscles on the bones and weight-bearing exercise also stresses bones, which keep them strong.
4. Consider supplements. If you can't get enough calcium from food or sunshine, take a daily supplement that includes 1,000 milligrams calcium and 400 I.U. (international units) of vitamin D. But don't take it all at once: The body can only absorb 500 milligrams of calcium at a time.
5. Get a bone density test. A bone mineral density test – a DEXA scan, or dual-energy X-ray absorptiometry – will show how your bone mass is holding up. The NOF advises women older than 65, and those with risk factors (like thinness, family history, history of fractures) to get one earlier. Because bone loss accelerates after menopause, doctors also recommend getting a baseline bone scan, especially if you’re not planning to take estrogen. At the very least, discuss the test with your doctor.
6. Move to medications. If you have osteopenia or osteoporosis, discuss drug therapy with your doctor. Medications include biphosphonates (alendronate, risedronate and ibandronate), raloxifene, calcitonin, teriparatide and estrogen/hormone therapy. Biphosponates, the most widely used medication for osteoporosis, increase bone mass and reduce the incidence of spine, hip and other fractures.
But they have drawbacks: They’re tough to swallow and hard on the GI tract, leading to heartburn and gastric ulcers. Some meds can be given intravenously, but they can cause side effects such as flu-like symptoms, muscle and joint pains and headaches. 7. Protect yourself from falls. Remove slippery area rugs, salt icy pathways, wear snow and ice traction cleats on your shoes (buy them online or at sporting stores) – and use a cane or walker if you need one. This won't keep you from getting osteoporosis. But given the devastating repercussions of hip fractures, it doesn't hurt to skid-proof your house. 7 Best Bone Building Foods
1. Seeds
Think of bone-building minerals and calcium first comes to mind. Our skeleton is largely made of calcium, but other minerals play a key role too. In fact, 50% of the body’s magnesium resides in our bones. Low levels are linked to fragile bones and calcium loss, research shows.
All seeds are good magnesium sources, but pumpkin seeds outshine the rest.
Here are a few ways to eat seeds:
2. Nuts
Bones aren’t hard and brittle; they’re living organs with live cells and fluids. Every day, bone cells break down and build up. That’s how they remain strong and heal after a break.
Walnuts – rich in alpha linolenic acid, an omega-3 fatty acid – decrease the rate of bone breakdown and keep bone formation constant, according to a 2007 Nutrition Journal study. Brazil nuts are also great sources of magnesium.
So grab a small handful for a snack or sprinkle a couple tablespoons into your oatmeal. Keep in mind that nuts are high-fat and high-calorie, so limit your daily serving to one ounce – about 1/4 cup. Other foods with alpha linolenic acid include: flaxseed oil, ground flaxseeds, walnut oil, soybeans, soybean oil and canola oil.
3. Tap Water
Fluoride, famed for its role in preventing cavities, is also a component of your bones and adds to their density. Many communities add this mineral to drinking water to help dental health. So if you drink only bottled water, you may not get enough fluoride to protect your teeth or bones.
4. Leafy Greens
Make green your new favorite color. Your salads and steamed greens are packed with bone-building nutrients, particularly calcium, magnesium and vitamin K.
Vitamin K is critical in forming bone proteins and cuts calcium loss in urine. Too little of this fat-soluble vitamin increases risk of hip fractures, research shows.
Just one cup of raw or a half-cup of cooked greens provides several times the recommended intake of 90 micrograms per day. Here are a few ways to sneak some extra greens in today:
5. Beans
Have beans for supper tonight, especially pinto, black, white and kidney beans. You’ll get another good boost of magnesium and even some calcium. The U.S. Dietary Guidelines for Americans recommends at least 2-1/2 cups of beans and other legumes (peas, lentils) weekly.
Bean-eaters reduce their risk of cancer, heart disease and obesity. Problem is, most people don’t know what to do with them. Here are a few ideas:
6. Fish
When it comes to bones, calcium is nothing without vitamin D, which we need so our bodies can absorb calcium. As with vitamin K, vitamin D deficiency also is linked to hip fracture. In fact, 50% of women with osteoporosis who were hospitalized for hip fracture had signs of vitamin D deficiency, according to a scientific review by the American Medical Association.
The best fish? Salmon. A small serving of salmon – only 3-1/2 ounces – gives you 90% of the daily recommended amount of vitamin D. If you want a double-whammy of bone-building nutrients, don’t just look to fresh fish. Canned salmon provides vitamin D and calcium… as long as you eat the bones. (Don’t worry, they’re soft.)
7. Dairy
Many of us forget about milk once we outgrow crazy straws and strawberry powder, but bones don’t stop developing in our teens. We add bone mass even in our 20s, but only if we consume enough of the nutritional elements.
Once we reach menopause and begin to lose estrogen, our bones lose calcium more rapidly than at any other time in our lives. Here again, calcium and vitamin D can help delay the loss of bone mass.
Milk is a good source of vitamin D because it is fortified. Cheese, yogurt and ice cream generally aren’t; they contain little vitamin D. Drink nonfat or 1% milk; the others have high saturated fat and cholesterol content. Pour a nice cold glass and enjoy – with or without a cookie.
No comments:
Post a Comment